Rotations at the Veterans Affairs Clinics have become a golden opportunity for Palmer students to give back, get hands-on and launch their careers.
As Peter Hibl, D.C. (West, ’18), rose early one morning in July 2018 to embark on the first day of his student rotation at the Veterans Affairs Palo Alto Health Care System, he was bringing home an ambition he’d been nurturing since the beginning of his time at Palmer.
At the same time, a new chapter was opening — one that would lead him across the country to the VA hospital in Buffalo, New York, for a one-year postgraduate residency and then all the way back to the Bay Area to reunite with his former attending, Robert Walsh, D.C. (West, ’95), as the newest member of the Palo Alto VA chiropractic program faculty.
Today, as he prepares to welcome, train and mentor his own Palmer College student on rotation, Dr. Hibl takes stock of where he’s been. “The clerkship was absolutely what laid the foundation for me,” he says from his car on the drive home from the clinic. “Now, I can’t help but feel the circle is being completed. Needless to say, I’m very excited.”
That’s a sentiment shared by Jennifer Steward, M.B.A., Palmer’s director of clinical and co-curricular programs. Steward oversees all of the College’s preceptorship programs, including the Department of Defense/Veterans Affairs (DoD/VA) rotations, which give students a unique opportunity to care for complex patients in a multidisciplinary setting while serving those who have served our country. As part of that role, she’s responsible for helping connect the right students with the right clinics, setting the stage for productive, lasting relationships.
“It’s a stringent vetting process,” Steward explains from her office on Brady Street in Davenport. Early on, she sits down with every student who applies for a rotation to understand their motivations and whether the program is a fit. Once Steward has screened the applicant pool, the program’s affiliate doctors review profiles, interview students and, ultimately, make offers. “I think we’ve had really nice pairings,” she says. “And now to be at the point where some of our recent graduates have been hired and are starting to take on students themselves — it’s a really neat cycle.”
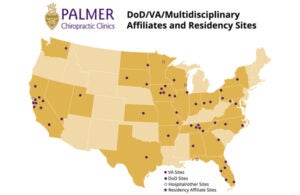
The rotation program, which began in 2007, has grown considerably since Steward assumed her role in 2018. In those short years, the number of VA hospitals, DoD sites and other multidisciplinary affiliates hosting students has more than doubled from 23 to 50 (most of them VA), while the number of Palmer students participating in rotations each year has climbed from 26 to 44. In fact, the College is on track for record participation in 2021, with 30 students from all three campuses already headed for rotations as the fiscal year kicked off this summer. Of those 30 students, six are representing Palmer College at four affiliate sites for the first time ever.
 As more and more VA centers bring chiropractic care on-site — all VA clinics must offer it themselves or partner with a community clinic — Steward has noted an uptick in the volume of referrals to the Palmer program. “A lot of the doctors within the VA system know each other, so the positive buzz gets around.”
As more and more VA centers bring chiropractic care on-site — all VA clinics must offer it themselves or partner with a community clinic — Steward has noted an uptick in the volume of referrals to the Palmer program. “A lot of the doctors within the VA system know each other, so the positive buzz gets around.”
In fact, Steward has her pick of rave reviews from affiliate doctors, who cite everything from the specific techniques and clinical knowledge with which Palmer students come equipped to their independence and leadership abilities. One chiropractor at the VA hospital in Fargo, North Dakota, described how the Palmer student at his clinic was able to help train students from other chiropractic colleges on the same rotation. “He’s teaching the other students what it’s like to be advanced to his level after only one trimester at the VA,” he wrote.
Of course, the DoD/VA rotation is fundamentally an opportunity for Palmer students to learn, which is what makes it such a profoundly rewarding experience for the high-achieving students who earn a place in the program. According to the 2020-2021 numbers, which account for reduced patient volumes due to COVID-19, participants had an average of 269 patient encounters each — 28% more than the minimum required for graduation.
“I don’t think there was one day during my clerkship that I didn’t grow at least a little bit,” says Dr. Hibl. “At the end, you’re a much more competent clinician. You leave ready for private practice.”
Or, like Dr. Hibl himself, you leave ready to deepen your training with an extremely competitive postgraduate VA residency.
For Charbel Medlej, D.C. (Main, ’20), two VA rotations — one in Tuscaloosa, Alabama, the other in Pittsburgh, Pennsylvania — left him craving more.
“My rotations taught me how to be a forever student,” Dr. Medlej says from the VA hospital in Canandaigua, New York, where he’s wrapping up his residency and preparing for his new job at the Hunter Holmes McGuire VA medical center in Richmond, Virginia. “It’s about showing up with an open mind, willing to learn. Even as a clinician, you’re never going to have all the answers, so you have to be comfortable with being uncomfortable and continue to grow by searching for answers each day.”
Ultimately, a fine balance of both clinical excellence and a readiness to adapt is required to serve the patients who come to VA medical centers for care. Often considered “complex,” many of these patients have been dealing for years with pain, functional limitations and other health issues, including psycho-social factors that, in Dr. Medlej’s words, can “muddy the waters.”
“Veterans have been through things most of us haven’t,” says Dr. Medlej. “A lot of them have seen combat deployments, and what they’ve been exposed to — both physically and psychologically — contributes to their conditions today. Everyone’s pain experience is unique, and we have to emphasize a biopsychosocial approach to managing it. That challenge has made me a better clinician.”
So has working as part of a team of multidisciplinary health care providers, a necessary approach for effectively managing these complicated presentations. For the chiropractic students on rotation, the chance to collaborate in an integrated setting and learn from a broad range of medical professionals is an invaluable aspect of the program.
Mariah Hargrove, D.C. (Florida, ’21), spent much of her rotation at the VA in Little Rock, Arkansas, working on an interdisciplinary team in the Integrated Medicine Pain Alternative and Complementary Treatment — or IMPACT — clinic. There, she found herself surrounded by an array of knowledgeable providers: an acupuncturist, a nutritionist, a primary care physician, a physiatrist, yoga and tai chi instructors and, of course, her attending chiropractor. Every week, the team came together to discuss what each patient needed in order to get off pain medication.
“Of course, I think chiropractic is the best — that’s why I went to Palmer,” says Dr. Hargrove, who was the first-ever chiropractic student to rotate at the Little Rock VA. “But when you get into a setting like this, seeing people who’ve had significant injuries or been in pain for 20 years, you realize you’re simply not always going to be the be-all and end-all. Working together with those other practitioners and understanding their point of view was eye-opening.”
The compliment goes both ways, according to Dr. Medlej. “Students who talk to me about this program want to know if chiropractors are respected in the VA,” he says. “I tell them I think chiropractors have absolutely earned the esteem of other providers.”
Dr. Hibl recalls a pivotal moment during his student rotation, working alongside a medical student intern on a patient with shoulder pain. “I realized that our knowledge and skills in that situation were right on par with each other,” he says. “And that intern saw what a broad knowledge chiropractors can have.”
“Palmer gives us a great background in all-around patient care,” adds Dr. Hargrove, who spent six months in the Palmer clinic before her rotation. “Taking patient histories, doing exams, adjusting — even though the patient base was different and more complex in the VA setting, my framework stayed the same. I did what Palmer taught me.”
What she could only truly learn through the rotation, though, was how to care not for patients but for people.
“I had patients who would say, ‘I’m sorry if I get a little irritated. It’s just because I’m in pain,’” Dr. Hargrove says. “Everyone was so friendly and open. I really learned communication skills and how to deal with conflict. I feel like I came out a more well-rounded person.”
Busy sorting out her license and applying for jobs at VA centers around the southeast, Dr. Hargrove is carried by the relationships she forged on her rotation. “The people are what made me want to stay in the VA,” she says, referring to the care teams she worked with, the attendings who mentored her and the patients she’d come to know.
Dr. Hargrove recalls the emotional goodbyes she exchanged with those patients in the final days of her rotation. “‘Are you sure you have to leave?’ they kept asking me. ‘You don’t want to stay?’ To see that I really did make a difference for these people who sacrificed for our country — it was so fulfilling to be able to say I helped them get better.”
READ MORE from Palmer Proud Magazine
 As more and more VA centers bring chiropractic care on-site — all VA clinics must offer it themselves or partner with a community clinic — Steward has noted an uptick in the volume of referrals to the Palmer program. “A lot of the doctors within the VA system know each other, so the positive buzz gets around.”
As more and more VA centers bring chiropractic care on-site — all VA clinics must offer it themselves or partner with a community clinic — Steward has noted an uptick in the volume of referrals to the Palmer program. “A lot of the doctors within the VA system know each other, so the positive buzz gets around.”